Immunotherapy in Turkey
Immunotherapy in Turkey is an article that aims to give you all the information you do not know about Immunotherapy in Turkey and more. We kindly shared the main headings with you;
What is immunotherapy?
One type of treatment for cancer is immunotherapy. To strengthen the immune system and assist the body in locating and eliminating cancer cells, it makes use of chemicals produced by the body or in a laboratory. Many different cancers can be treated using immunotherapy. It may be utilized both independently and in conjunction with other cancer therapies such as chemotherapy.
Which types of cancer can immunotherapy treat?
Immunotherapy in Turkey treats many health conditions however it is typically suggested for people with advanced cancer. Immunotherapy in oncology aims to manage the disease. Immunotherapy may also be used to treat additional cancer types, such as:
- Liver cancer
- Stomach cancer
- Breast cancer
- Cervical cancer
- Bladder cancer
- Lymphoma
In some circumstances, immunotherapy may be used to lower the chance of relapse in patients whose non-metastatic cancer has been cured. This is more common in lung cancer and in some melanomas. Immunotherapy may also be used in conjunction with chemotherapy, depending on the type of cancer.
How immunotherapy treats cancer?
Your body uses a sophisticated system called immune system to combat cancer. Cells, organs, and proteins are all involved in this process. However, cancer cells can find ways to avoid immune system destruction, despite the fact that the immune system can stop or reduce cancer progression. Cancer cells, for instance, could:
- Possess genetic alterations that reduce their immunological visibility.
- Possess surface proteins that inhibit immune cells.
- Alter the healthy cells around the tumor so that they obstruct the immune system’s ability to combat the cancer cells.
Several of the immune system’s natural defenses are frequently overcome by cancer, allowing cancer cells to spread and reproduce. Various immunotherapy treatments operate in multiple ways. Some immunotherapy procedures assist the immune system in halting or reducing the growth of cancer cells. Others aid in the immune system’s destruction of cancer cells or prevent the disease from spreading to other bodily areas.
For instance, immune cells are sometimes observed in and surrounding tumors. These lymphocytes, also known as tumor-infiltrating lymphocytes, or TILs, are evidence that the immune system recognizes the tumor. Individuals who have cancers that have TILs frequently fare better than those whose tumors do not.
Invest in your health, invest in a brighter future. Our comprehensive medical programs deliver real results, while you indulge in the beauty and serenity of our destination.
Who are the ideal patients for immunotherapy?
The type and stage of your disease, the biomarkers it expresses, and whether immunotherapy is now recommended for use in certain cancer treatment scenarios will all determine whether you would be a candidate for it. Immunotherapy may be appropriate for you if:
- Biomarkers that are positive for PD-L1 expression, high microsatellite instability, or high tumor mutational load are discovered through genomic analysis.
- Your cancer has progressed. In general, once traditional treatment options have been explored, you may be admitted into a clinical trial testing an immunotherapy drug’s effectiveness against your specific cancer type or against genetic markers found in its DNA.
- You are suffering from non-small cell lung cancer, particularly if it has spread or is advanced in the stage. The recommended treatment for this form of cancer now includes genomic testing. According to studies, people with advanced non-small cell lung cancer who benefit with immunotherapy live longer than those who do not. Some people have been taking maintenance doses for a while.
What is genomic analysis?
Treatment methods may alter from a one-size-fits-all approach to more targeted techniques as we understand the biology of cancer tumors and how their unique biomarkers may respond to immunotherapy. Doctors may someday base their recommendations on whether specific genomic alterations detected in cancer’s DNA are more likely to respond to a form of treatment, such as a particular immunotherapy medicine, rather than the location of cancer (for example, breast cancer, or pancreatic cancer).
Advanced genomic testing may be the initial step if your oncologist decides you might be a candidate for immunotherapy. The DNA from cancer tumor cells is analyzed using these high-tech methods to seek specific biomarkers that indicate particular genetic mutations (changes) that may be linked to medicines that have been successfully used for those mutations.
How immunotherapy is administered?
Various immunotherapy treatments can be administered in various ways such as,
- Intravenous (IV): Immunotherapy is administered into veins via injections.
- Oral: You ingest the immunotherapy pills or capsules.
- Topical: You apply the immunotherapy cream directly to your skin after purchasing it. Skin cancer that has just started can be treated with this kind of immunotherapy.
- Intravesical: The immunotherapy enters the bladder right away.
What are the types of immunotherapy?
If you receive immunotherapy in Turkey several variables will affect the kind of immunotherapy, dosage, and timing your doctor prescribes. The cancer’s size, location, and extent are a few of these factors that can be considered. Further significant factors include your age, general health, weight, and any potential adverse effects. Discuss with your doctor the reasons for their recommendation of a particular immunotherapy type for you.
Remember that any new adverse effects must be reported as soon as possible to a member of your healthcare team. Treatment may need to be halted if major adverse effects do arise, and your immune system may need to be suppressed with large doses of corticosteroids.
To learn more about the cost of immunotherapy in Turkey, continue reading.
Immune checkpoint inhibitors and monoclonal antibodies
The immune system produces antibodies when it recognizes a threat. Proteins known as antibodies bind to antigens to combat infection. The immunological response in your body is triggered by substances known as antigens. In a lab, monoclonal antibodies are created to supplement or replace the body’s own antibodies. Monoclonal antibodies, mAbs in short, have several types like naked monoclonal antibodies, conjugated monoclonal antibodies, and bispecific monoclonal antibodies.
Monoclonal antibodies can aid in the battle against cancer in several ways. They can be employed, for instance, to prevent abnormal proteins in cancer cells from acting normally. This is also regarded as a sort of targeted therapy, which is a method of treating cancer with drugs that specifically target the genes, proteins, or tissue environment that supports the growth and survival of the tumor.
Some monoclonal antibodies work by blocking or preventing immunological checkpoints to strengthen your immune system. The body employs immunological checkpoints to automatically halt immune responses and stop the immune system from attacking healthy cells. These checkpoints can be activated by cancer cells to help them conceal themselves from the immune system.
Side Effects
Monoclonal antibodies are administered into a vein via injections. As antibodies are proteins, administering them occasionally results in allergic reactions. The potential negative consequences can be listed as follows:
- Fever
- Chills
- Weakness
- Headache
- Nausea
- Vomiting
- Diarrhea
- Reduced blood pressure
- Rashes
Naked mAbs typically have less severe adverse effects when compared to chemotherapeutic medications. Nonetheless, some people may still experience issues as a result. The antigens they target can have an impact on some mAbs’ adverse effects. For instance:
- A mAb called bevacizumab (Avastin) targets a protein called VEGF that influences the development of tumor blood vessels. High blood pressure, hemorrhage, inadequate wound healing, blood clots, and renal damage are some of the possible side effects.
- An antibody called cetuximab (Erbitux) targets the EGFR cell protein, which is present in healthy skin cells (as well as some types of cancer cells). Some persons who use this medication may get severe rashes.
Similar side effects also apply to immune checkpoint inhibitors. Although the following are observed less often, regarding immune checkpoint inhibitors you may also experience,
- Infusion responses: Some individuals may experience an infusion response when receiving these medications. This might cause symptoms similar to an allergic reaction, such as a fever, chills, facial flushing, rash, itchy skin, feeling lightheaded, wheezing, and breathing difficulties.
- Autoimmune responses: These medications take away one of the immune system’s defenses by targeting a checkpoint protein. Sometimes the body’s immune system reacts by attacking other organs or tissues, which can result in significant or even fatal issues with the kidneys, liver, lungs, intestines, liver, or other organs.
Non-specific immunotherapies (Immunomodulators)
Cancer cells are destroyed by non-specific immunotherapies, often known as non-specific immunomodulating drugs. Non-specific immunotherapies come in a variety of forms such as Cytokines and Bacillus Calmette-Guerin (BCG) and function differently:
Cytokines. A component of the immune system is cytokines. These are proteins that communicate with one another in order to stimulate the immune system. Two categories of cytokines are employed in the treatment of cancer:
- Interferons: Your immune system creates these proteins to inform your body that a pathogen, usually a virus, is present. To aid your immune system in fighting cancer, interferons can be created in a laboratory. They may also prevent the development of cancer cells. Side effects caused by interferons are low white blood cell counts, flu-like symptoms, rashes of the skin, and thinning hair.
- Interleukins: Proteins called interleukins are used as messengers by cells. They also trigger an immunological reaction. For instance, melanoma and kidney cancer can be treated using laboratory-produced interleukin-2 (IL-2) or aldesleukin (Proleukin). IL-2 therapy frequently causes weight gain and low blood pressure as side effects. Moreover, some patients report flu-like symptoms.
Bacillus Calmette-Guerin (BCG). Similar to the microorganisms that cause tuberculosis, this type of immunotherapy. It is used for the treatment of bladder cancer. With a catheter, BCG is inserted directly into the bladder. It adheres to the bladder’s interior lining and triggers the immune system to eliminate cancerous cells. BCG treatment may result in flu-like symptoms, including fever, chills, and exhaustion. Moreover, it may result in bladder burning. By injecting BCG right into the tumors, certain melanoma skin cancers might also be cured.
Oncolytic virus therapy
Oncolytic virus therapy, also referred to as virus therapy, employs viruses that have been altered in a lab to kill cancer cells. A virus that has undergone genetic modification is introduced into the tumor. When the virus enters the cancer cells, the virus replicates itself. The cancer cells, therefore, explode and die. When a cell dies, it releases proteins that cause your immune system to begin attacking any cancer cells in your body that have the same proteins. The virus stays outside of healthy cells.
Side Effects
Chills, fatigue, flu-like symptoms, soreness at the injection site, nausea, and fever are a few examples of frequent adverse effects linked to the oncolytic virus.
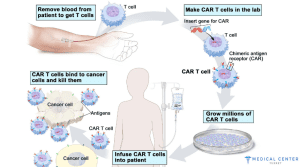
T-cell therapies
T cells are immune cells that combat infection. T cells are drawn out of the patient’s blood during T-cell treatment. The cells are then given specific proteins, known as receptors, in a laboratory. These T cells can identify cancer cells thanks to the receptor. The body receives the modified T cells back. When they arrive, they locate and eliminate cancer cells. Chimeric antigen receptor (CAR) T-cell therapy is the term used to describe this sort of treatment. Fever, confusion, low blood pressure, and, in rare cases, seizures are just a few of the side effects. Some blood malignancies can be treated using CAR T-cell therapy. This kind of therapy and other approaches to altering T cells to treat cancer are still being researched by researchers.
Side Effects
CAR T-cell treatment can be very effective against some types of hard-to-treat tumors, but it can also sometimes induce serious or even life-threatening side effects. Because of this, it must be administered in a hospital that has received specialized training in its administration, and patients must be constantly monitored for a number of weeks after receiving the CAR T cells.
The possible complications can be listed as follows,
Cytokine release syndrome (CRS): As CAR T cells proliferate, they have the potential to release vast quantities of the cytokines into the blood, which can boost the immune system. This release’s potentially harmful negative effects include:
- High fever and chills
- Difficulty in breathing
- Extreme nauseousness
- Vomiting
- Diarrhea
- Fainting
- Dizziness
- Headaches
- Rapid heart rate
- Exhaustion
- Joint and/or muscle aches
Nervous system issues: This therapy might occasionally have negative effects on the nervous system, resulting in symptoms like:
- Headaches
- Alterations to awareness
- Uncertainty or agitation
- Seizures
- Trembling or shaking (tremors)
- Difficulty in comprehending and speaking
- Loss of balance
Apart from the above-listed side-effects, you may get affected by,
- Allergy symptoms after the infusion
- Abnormal blood mineral levels, such as low levels of potassium, sodium, or phosphorus
- A weakened immune system that increases the chance of developing serious infections
- Low blood cell counts increase the likelihood of infections, exhaustion, and bleeding or bruising
Adult patients are often advised not to drive, operate heavy machinery, or engage in any other potentially hazardous activities for at least a few weeks following treatment due to the risk of these adverse effects. Any negative effects from CAR T-cell therapy must be immediately reported to your medical staff because there are frequent medications that can help address them.
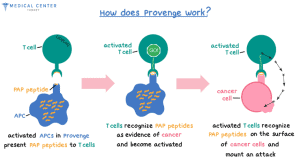
Cancer vaccines
A cancer vaccine can aid your body’s immune system. Your immune system gets exposed to a foreign protein, known as an antigen, through vaccination. This prompts the immune system to identify and eliminate that antigen or associated compounds. Adjuvants, which are frequently used in vaccine formulations, serve to further increase the immunological response. The immune system attacks cells that contain one or more specific antigens as a result of cancer vaccinations. The immune system possesses memory-specific cells, thus it is hoped that the vaccination will continue to function for some time after being administered. Cancer vaccines come in two varieties: those used for prevention and those used for treatment.
- Cervical, anal, throat, vaginal, vulvar, and penile cancers have all been related to specific strains of the human papillomavirus (HPV). In actuality, HPV infection is the main cause of cervical cancer. Gardasil, a vaccine against the human papillomavirus (HPV), a virus that can cause particular types of cancer, is one example of a cancer prevention vaccine.
- One example of a therapeutic vaccination includes spuleucel-T (Provenge), which treats advanced prostate cancer that does not respond to hormone therapy. The most common moderate side effects are headache, nausea, back and joint discomfort, weariness, fever, chills, and chills. Some men may experience more serious symptoms, such as breathing issues and high blood pressure.
- T-VEC is regarded as a cancer vaccine as well. It is a vaccination for treating advanced melanoma skin cancer. It is generated from a herpes virus that has been modified in a lab to produce a chemical called a cytokine, which the body usually makes. This cytokine strengthens the immune system and briefly mimics flu symptoms.
How regular the treatment is performed?
Your immunotherapy regimen’s frequency and duration are determined by:
- The type and stage of your disease
- The type of immunotherapy you receive
- How your body responds to treatment
Depending on these factors you can receive care every day, every week, or every month. Some immunotherapies are administered in cycles. A cycle consists of a treatment phase and a recovery phase. Your body can repair, respond to immunotherapy, and create new, healthy cells during the period of rest.
What are the advantages of immunotherapy?
There are several potential advantages to immunotherapy. Immunotherapy,
- Increases the likelihood that many cancers will survive over the long run.
- Destroys several tumor kinds and, in many circumstances, can stop tumors from coming back.
- Help stop the spread of a variety of cancers.
- Boosts your immune system so that it can continue to fight cancer long after therapy has ended.
- Causes adverse effects that, on the whole, are less severe than those brought on by more conventional cancer treatments like chemotherapy. To decide if immunotherapy is the best course of treatment for you, go over the advantages and disadvantages of the therapy with your doctor.
Does FDA approve immunotherapy drugs?
Not all cancer types can be treated with immunotherapy. Before a therapy is established as standard of care, researchers must demonstrate that it is at least as successful as the currently accepted therapies. As those malignancies had more extensive long-term data, melanoma and non-small cell lung cancer were the first cancers to receive FDA approval for immunotherapy treatment. Interleukin-2 (IL-2) and interferons were the main treatments for these tumors up until roughly five years ago (cytokines). Immune checkpoint inhibitors are increasingly often employed today. Immunotherapy has not been expressly approved by the FDA for colon and pancreatic cancer.
What is the cost of immunotherapy in Turkey?
You may ask yourself “What is the cost of immunotherapy in Turkey?”. Just like in any case with oncological treatments, the cost of immunotherapy in Turkey depends on many factors such as the therapy treatment types you receive, which medications you take additionally, how frequent are your check-up sessions, and how effective is the treatment for you. Immunotherapy comes in a wide variety of forms, and each type can be very expensive. The cost of immunotherapy in Turkey is more than $100,000 per patient and is generally quite expensive.
Immunotherapy in Turkey Summary (Price, Duration Time, Hospitalization)
| Operation Number | Depends on the condition of your state and the effectiveness of previous operations | Time to return to work | Few weeks, consult your doctor |
| Operation Time | – | Recovery | 3 days |
| Anaesthesia | – | Persistence of Results | 5+ years |
| Sensitivity Time | Few weeks, consult your doctor | Hospital Stay | – |
| Price | Starting from 100,000 EUR | ||